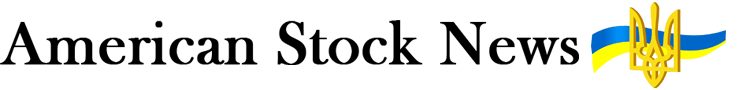
His initial written presentation of the breakthrough, ‘Über eine neue Art von Strahlen’ (‘About a new kind of ray’), was published the following month. It described a new kind of radiation, which he referred to as ‘X-rays’ with the X indicating that the type of radiation was previously unknown. The X-ray name stuck, and his surname was subsequently adopted as the internationally recognized unit of measurement for ionizing radiation (the Röntgen).
If you hold your hand between the discharge device and the screen, you can see the darker shadows of the bones of the hand.
Wilhelm Röntgen
‘Über eine neue Art von Strahlen’ (‘About a new kind of ray’), published in 1895.
Röntgen’s discovery started a revolution in medical imaging that continues to play an important role in healthcare today. X-ray based diagnostic imaging is a cost-effective and straightforward technique that is widely used by radiologists to identify and assess fractures, infections, tumors, bone abnormalities, and trauma. Ever since its underlying discovery in 1895, X-ray technology has made tremendous progress in improving diagnostic imaging and patient care – something Philips continues to pioneer to this day.
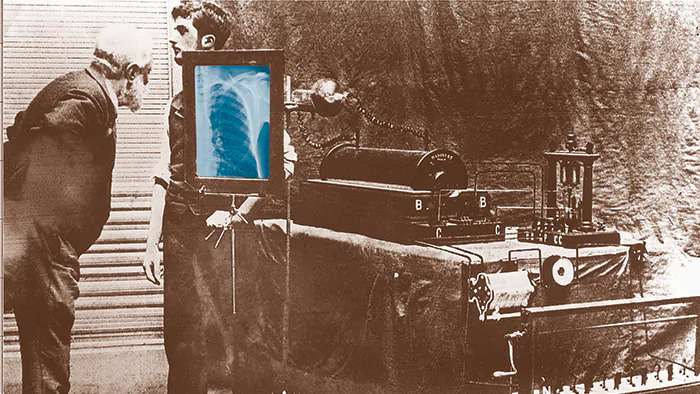
Early days
Every child knows that you can create much better hand shadow puppets when the sun is shining than when it is cloudy, because hand shadow images work best when you have a bright single-point light source. The same is true for X-ray imaging, only this time you need body-penetrating X-rays, not light, to perform the trick. Right from the start, Philips saw the potential.
A suitable X-ray source (X-ray tube) is little more than a glass vacuum bottle with two metal electrodes in it, one of them heated (the hot cathode) so that it ‘boils-off’ electrons. Put a high enough voltage between the electrodes and the electrons accelerate towards the second electrode (the anode) hitting it with enough energy to create X-rays.
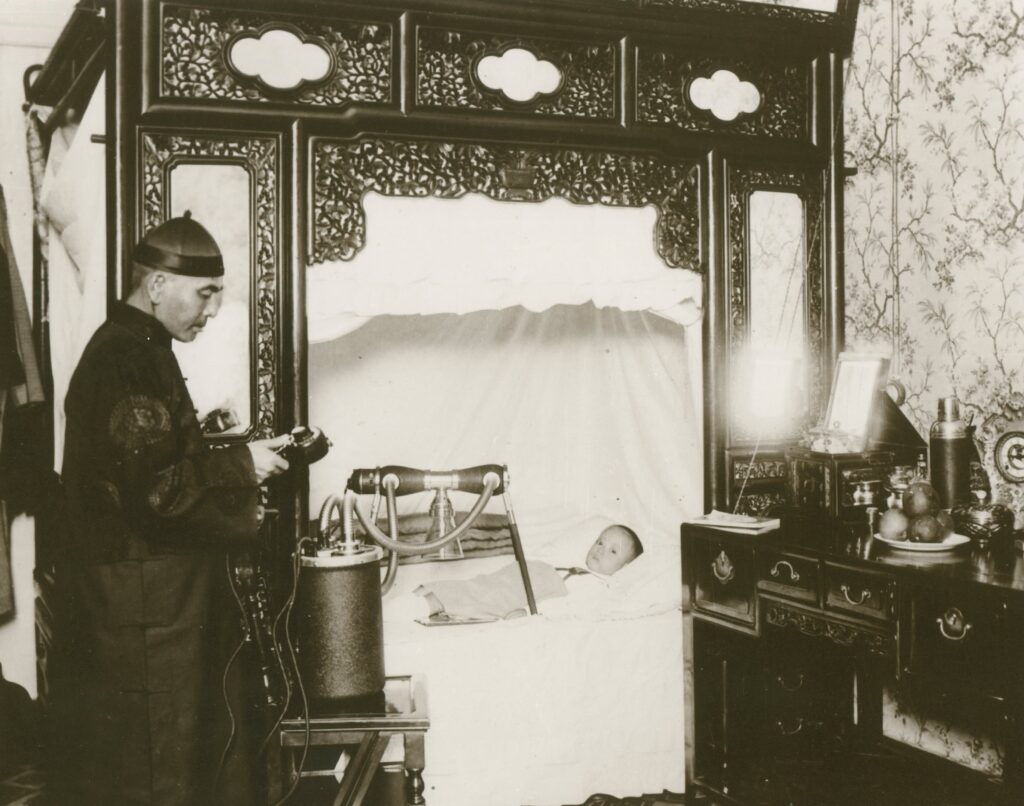
Having repaired X-ray tubes during the First World War at the request of Dutch physicians, something that drew on its expertise in manufacturing glass light bulbs, Philips began small-scale manufacture of its own X-ray tubes in 1919. Recognizing the possibilities in medical imaging, it went on to acquire German company C.H.F. Mueller, an existing X-ray tube manufacturer that had unique expertise in focusing X-rays in the direction you want them to go. Coupled with Philips’ own technology to shield against stray radiation, it delivered exactly what was required for medical imaging – a focused X-ray beam that could be directed at the patient without risking long-term radiation exposure to radiologists. From there, Philips went from strength to strength in terms of its commercial offerings, delivering the first portable X-ray machine, the first high-power rotating anode X-ray tube, the first X-ray image intensifier for rapid viewing, and the first C-arm machine for easy image capture. To this day, the Röntgenstraße site on which the first Philips/Mueller joint venture was built remains a core element in Philips’ healthcare innovation ecosystem, housing both its Hamburg research laboratories and its DACH headquarters.
While steady progress in X-ray imaging continued over the years, it was not until the 1970s, with the introduction of affordable computing power and digital storage, that things really took a quantum leap forward. And once again, Philips was in the vanguard of this change.
From blurry images to precision diagnosis
With computing power came Computed Tomography (CT), a technique that uses a narrow X-ray beam to capture multiple images from different angles, which can be processed by a computer to build up incredibly detailed cross-sectional images (slices) of a patient’s internal anatomy. Philips quickly became a pioneer in CT imaging with several world-firsts, notably in the development of innovative solid-state X-ray detector technologies that progressively improved image quality while at the same time reducing X-ray dose. It also pioneered Spectral CT, a technique that delivers high diagnostic quality at low contrast agent dose, bringing CT’s diagnostic capabilities to vulnerable patients, such as those with reduced renal function, who cannot tolerate normal contrast agent doses. Philips’ latest development is a Spectral Photon-Counting CT (SPCCT) detector that allows CT scanners to perform molecular (functional) imaging, taking CT from today’s black-and-white images to color images in which different colors represent specific chemical elements. Over the years, CT imaging has enabled unprecedented improvements in precision diagnosis, something that Philips remains committed to for the future.
Interventional procedure imaging
While CT scanners are an excellent tool for precision diagnosis, they are typically not suitable for use during live interventional procedures such as catheterizations to unblock coronary arteries (angioplasty). So once again, Philips developed innovative new X-ray solutions. In 1981, for example, it introduced digital subtraction angiography, which subtracts dense (radiopaque) structures such as bone from a low-dose X-ray image to allow the detailed visualization of blood vessels, paving the way for many new interventional procedures, notably in cardiology. By then, Philips was delivering real-time image acquisition at up to 60 images per second.
From 2D to 3D image guidance
While the 2-dimensional images generated by conventional X-ray imaging are extremely useful, there are occasions when you want 3-dimensional images of a patient’s internal organs – what you would see if you physically opened them up to take a look. In 1992, Philips used its C-arm X-ray machine technology to perform Rotational Angiography (RA), in which a series of images is captured as the C-arm rotates around the patient. Viewed in a loop, these images create the impression of a 3D view.
The system worked well for high contrast structures, but still didn’t image soft tissue in sufficient detail. That left expensive MRI or CT imaging as the only option, with neither modality really being economically or workflow friendly enough to be used in the sort of image-guided minimally-invasive procedures carried out in cath labs. To solve the problem, Philips designed the XperCT – an X-ray system that uses technology to generate CT-like images, first introducing it to the market in 2005.
Enabling next-generation minimally-invasive procedures
With an economically viable, workflow friendly solution for interventional imaging in place, image-guided minimally-invasive surgery really took off, notably in cardiology where it offered faster treatment for common cardiac conditions and an alternative to open-heart surgery for high risk patients. Today, it is used for a wide range of cardiac procedures, ranging from straightforward angioplasty to highly complex heart valve replacement and treatment for cardiac arrhythmias. To enable these complex procedures, Philips introduced an X-ray based real-time navigation system in 2007 that displays a 3D image of the patient’s heart on a computer screen, allowing catheters to be precision guided to the right location in the heart. It was followed in 2017 by Philips’ Azurion with ClarityIQ technology – a fully integrated next-generation image-guided therapy platform that combines planning and navigation software with interventional devices such as catheters, plus the benefits of high image quality at ultra-low X-ray dose.
AI assisted workflows for lower cost of care
125 years after their discovery, X-rays continue to play an important role in Philips’ diagnostic and interventional imaging portfolio, adding critical information to the plethora of data needed for precision diagnosis, evidence-based decision making and targeted treatment. So much so that clinicians can sometimes find themselves with too much data and not enough time. Interpreting the data in ways that help clinicians to make better informed decisions and cope with increasing workloads is where Philips is employing artificial intelligence (AI) to advantage. This is typified by its latest IntelliSpace AI Workflow Suite platform, which orchestrates and transfers imaging, clinical and administrative data between devices and AI applications, enabling the deployment of multiple AI applications on a single platform. Among others, dedicated IntelliSpace packages are available for data integration, visualization, and analysis; comprehensive patient-centric cancer care; and radiology research aimed at creating improved care pathways. Philips is even co-developing AI-based software to standardize the assessment of complex pulmonary cases associated with COVID-19.