As another wave of mass COVID-19 infections spreads across the globe, healthcare workers and health systems have again been rapidly brought to the burst point. While there are regional and local differences in affliction and response, the numbers of people infected are soaring. With this, the numbers of deaths have also climbed. However, perhaps a sliver of a silver lining is that investigators have shared their learnings from last spring, and pharmacotherapy regimens have helped speed recovery. And soon COVID-19 vaccines, now successfully emerging from phase 3 trials, will become a clinical reality. Combined with the recent approval of an at-home testing kit, the pandemic may enter a new phase.
Notwithstanding these developments, much remains unknown about SARS-CoV-2 infection, such as why some people develop serious COVID-19 infections, versus others who don’t, and what the long-term consequences are for those infected. Regarding the former, new reports continue to emerge, such as those linking anticytokine therapies for inflammatory bowel disorders to potential COVID-19 protection, and the significantly worse prognosis for patients who develop pulmonary emboli. Regarding the long-term consequences, emerging reports highlight the early symptoms that portend the likelihood of patients having a case of COVID-19 that lingers far longer than that of most patients. Moreover, it is now clear that some of these patients not only have persistent symptoms like fatigue, but also chronic cardiac and other organ system disorders.
Concomitant with better management of the current surge and the impending deployment of vaccines, Chip Truwit, MD, FACR, Chief Medical Officer for Precision Diagnosis at Philips, sees the role of precision diagnosis ultimately evolving beyond the trenches of critical COVID-19 care and into a new role that helps health care providers better manage patients’ disease burdens, while also facilitating new research that will help influence how healthcare workers handle the next pandemic.
“Investigators have learned a lot about how to treat and manage COVID-19 patients in the past nine months,” Truwit said. “But it’s important that the medical and scientific communities do not stop learning about this disease and generating new data related to the pandemic – whether that’s through chest CT scans or anonymized ultrasound data in the cloud or looking at thrombi and correlating demographics with clinical outcomes. These kinds of data will be foundational to the population health studies that will drive advances in the future care of COVID-19. Additionally, we will eventually reach a phase where, for some cohort of patients, the consequence of COVID-19 becomes one of more chronic disorders, requiring on-going therapies. How rapidly the medical and scientific communities adapt to that reality will have significant impacts on patients, families, workplaces and societies.”

Philips worked intimately with customers
With its comprehensive portfolio of integrated radiology solutions, Philips has been supporting care providers as they diagnose, treat and monitor COVID-19 patients. From data-driven practice management and improving the radiology staff and patient experience, to increasing diagnostic confidence to improve patient care, Philips is connecting the right data, technology and clinical insights to enable the patient’s pathway through precision diagnosis and therapy. Philips worked intimately with customers to understand their challenges and meet their demands during the pandemic by ramping up production of Lumify, a hand-held point-of-care ultrasound solution with integrated REACTS tele-ultrasound capabilities for remote collaboration and training.
CT and diagnostic X-Ray are also critical in assessing COVID-related pulmonary damage, and the Philips team in the Philippines developed a novel solution to meet demand while keeping patients and staff as safe as possible. The team is converting industrial shipping containers into CT and X-Ray imaging cabins that can be located wherever they are needed – within hospitals, in hospital grounds, or out in the community.
Philips COVID-19 Recovery Toolkit
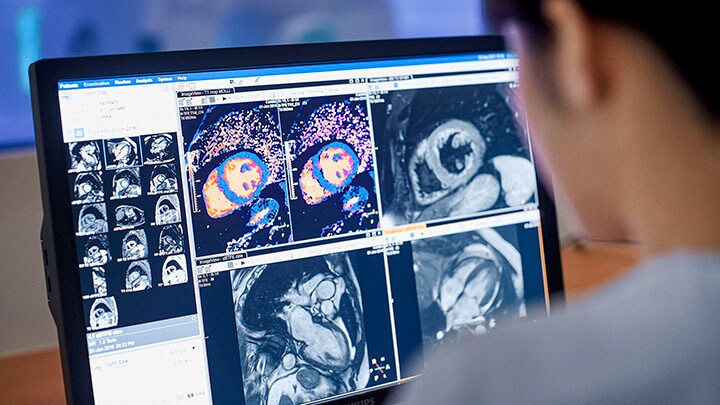
Now, this portfolio of solutions is primed to also help generate research insights, especially as solutions such as Philips Operational Informatics and the Philips COVID-19 Recovery Toolkit help bring patients safely back into healthcare facilities. For example, ultrasound, cardiovascular magnetic resonance (CMR) and spectral CT, integral to daily clinical practice, are already used in research studies to help differentiate the impacts of COVID-19-induced heart disease.
One of the biggest questions about the lasting effects of COVID-19 concerns heart damage in patients and the long-term effects. One recent study of patients who recovered from COVID-19 analyzed CMR images and saw that abnormal findings were present in 78% of patients, which the study authors said is indicative of myocardial edema and/or inflammation in most patients, and pericardial involvement in some. This heart damage may not have ever been discovered without this research; many of these patients reported only mild COVID-19 symptoms. Another recent research study analyzed CMR images in patients that recovered from recent COVID-19 and found that myocardial edema and late gadolinium enhancement (LGE) are common in COVID-19 convalescents, and that residual pulmonary disease was likely the driver of symptoms for these patients.
Cardiac ultrasound
Similarly, cardiac ultrasound is also helping reveal how COVID-19 damages the heart, which not only has the potential to help doctors more quickly identify patients who are at risk, but could also help guide future therapies. A recent study of hospitalized COVID-19 patients found that cardiac ultrasound (echocardiograms) can identify different types of post-cardiac injury structural damage that can occur in COVID-19 patients. Evidence of myocardial injury was present in 62% of the study population, and these patients had more electrocardiographic abnormalities as seen via ultrasound, such as higher inflammatory biomarkers, and an increased prevalence of TTE abnormalities than patients without heart injury.
Healthcare workers and health systems have also learned that COVID-19 patients could have variations in their physical status day-by-day, and that’s particularly true with cardiovascular status. A patient can have acceptable oxygen saturation levels one day, but then the next show a sharp decline. Patient’s characteristics, including age, weight and medical history are still poorly understood variables that influence cardiovascular response to COVID-19. Imaging solutions can help detect the structural abnormalities that inform care, while also helping connect the dots to outcomes.
“In the early days of the pandemic, when testing resources were unable to meet the demand, imaging played a vital role in the triaging of patients in many countries and communities. Additionally, imaging has been critical to the ongoing management of COVID-19 patients, both in the radiology department and in off-site locations including ICUs, emergency rooms, operating rooms and pre-hospital tents and cabins,” Truwit added. “The use of diagnostic imaging is not going to stop being used for COVID-19. I expect we will continue to see tremendous amounts of research develop as people have expanded the available data.”